Lymphovenous anastomosis (LVA)
Lymphovenous anastomosis (LVA) is a precisie supermicrosurgical technique (surgery on vessels less than 1 mm in diameter) aimed at decompressing a partially failing lymphatic system in patients with clinical signs of lymphoedema. During the surgery, working lymph vessels are found, which are then anastomosed under a microscope with selected venous vessels. As a result, lymphatic drainage from the lymphatic system into the blood system is achieved, thus “relieving” and decompressing the partially inefficient lymphatic system. The effects are already visible at the first control visit after a month


Who is a patient for LVA?
Patients are eligible for lymphovascular anastomoses if we are able to visualize active lymphatic pathways in previous imaging studies (lymphoscintigraphy, ICG imaging) and clinically the lymphoedema is at least minimally reversible in response to conservative treatment. Patients with secondary oedema are operated on after oncological, surgical and orthopaedic treatment, past trauma, as well as patients with primary oedema of undetermined aetiology. We perform the ICG examination on our own in Słupsk, for the lymphoscintigraphy the patient is referred to the Nuclear Medicine Department of the Polish Red Cross Maritime Hospital in Gdynia. In order to be eligible for surgical treatment, the patient must independently apply conservative lymphoedema treatment techniques and be directed and supervised for by a physical therapist.
How to assess the status of lymphatic duct damage? Am I eligible for LVA?
To assess the lymphatic pathways, the patient undergoes a physical examination and ICG lymphography is performed – see lymphography.
What does the LVA procedure technically consist in?
Intraoperatively, ICG lymphography is performed on a patient under general anaesthesia. On its basis the precise course of the lymphatic ducts and the zone of their damage related to the clinical symptoms of lymphoedema are determined. In selected 2-5 locations we make transverse incisions 3-5 cm long. In the subcutaneous tissue, we locate the appropriate venous vessels and then unobstructed lymphatic vessels. Lymphatic vessels and venous vessels are manually anastomosed. We place sutures on the subcutaneous tissue and skin. Similarly in each marked and incised area. The operated limb is then bandaged while still in the operating room.

How long does this surgery last? Is it burdensome for me?
The procedure takes between 2-6 hours, depending on the number of anastomoses performed. In order to shorten it, we work on two microscopes simultaneously. The treatment is not burdensome, the whole procedure is carried out in the skin and subcutaneous tissue. The patient suffers minimal pain and leaves for home on the first postoperative day.
Preparation for the procedure
- Dalacin C 300 mg three times daily – please start taking it 3 days before the surgery
- Before the surgery it is recommended to reduce the upper limb as much as possible (DLM). If the oedema is persistent, min. 3 days of Comprehensive Anti-Oedema Therapy
- Intensive work under supervision of a physical therapist on the limb in the 3rd and 2nd week before the surgery
- One week before surgery – compression therapy until surgery
- Please report to hospital with: blood group, blood tests: blood count, electrolytes, clotting times, creatine, chest X-ray
Post-operative care
Even before surgery, schedule (and possibly make) follow-up appointments 1,3,6,12 months after surgery!!!
Recommendations after LVA of the upper limb
(Elwira Wieczorek MA, Katarzyna Zubrewicz MA)
- Get plenty of rest during the first week after surgery.
- Daily disinfection of the surgical wound
- The dressings must be changed daily for 1 week.
- Showering is allowed, yet the wound cannot ‘soak’ in water
- Antibiotic for 7 days (Dalacin C 300 x 3/day)
- Bandage the arm at day 0 (Thuasne Biflexideal Short-Stretch compression bandage). If there is no specialist available who can show you how to self-bandage, 23-32 mmHg POST MASTECTOMY Compression Sleeve with Gauntlet (class 2) is recommended. An auto-adjustable nighttime compression sleeve (MOBIDERM® Autofit) is recommended at night. Attention: the wound must be completely healed or dressed while wearing the compression sleeve
- Physical therapy starting 2 weeks after the operation and after 3 weeks Manual Lymphatic Drainage is recommended bypassing the operated area.
- A grade 2 compression sleeve is recommended until approximately 6 months for a follow-up visit and potential ICG.
Recommendations after LVA of the lower limb
(Elwira Wieczorek MA, Katarzyna Zubrewicz MA)
- Get plenty of rest during the first two weeks after surgery.
- Daily disinfection of the surgical wound
- The dressings must be changed daily for 1 week.
- Showering is allowed, yet the wound cannot ‘soak’ in water
- Antibiotic for 7 days (Dalacin C 300 x 3/day)
- Bandage the arm at day 0 (Thuasne Biflexideal Short-Stretch compression bandage). If there is no specialist available who can show you how to self-bandage, 32-45 mmHg a compression stocking of 32-45 mmHg (class 3) is recommended. An auto-adjustable compression stocking (MOBIDERM® Autofit) is recommended at night. Attention: the wound must be completely healed or dressed while wearing the compression stocking
- Physical therapy starting 3 weeks after the operation. After 3 weeks Manual Lymphatic Drainage is recommended bypassing the operated area.
- A grade 3 compression stocking is recommended up to 6 months after surgery (of course it all depends on the type of lymphedema)

LVA involves the anastomosis of a lymphatic and venous vessel 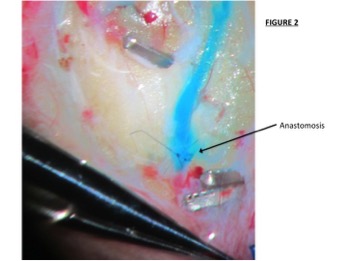
LVA involves the anastomosis of a lymphatic and venous vessel 
For LVA we use the world’s most precise set of Japanese supermicrosurgical instruments
